Shoulder Dislocation & Instability
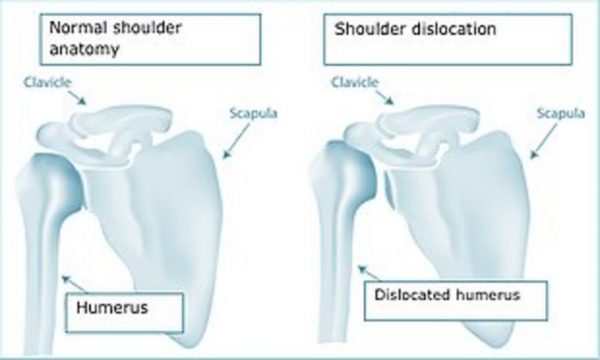
The shoulder is made up of a ball and socket joint – the ball-shaped head of the upper arm bone (humerus) articulates in the socket of the glenoid cavity of the shoulder blade (scapula). The ball and socket provides an excellent range of motion but this predisposes to dislocation.
Causes of Shoulder Dislocation
Trauma due to accidents with overhead or contact sports and workplace injuries may tear the constraints (ligaments) holding the humerus on the glenoid, causing a dislocation.
Symptoms of Shoulder Dislocation
A shoulder dislocation can be partial (subluxation) or complete with symptoms of:
- pain
- weakness
- numbness
- instability
The dislocation generally indicates ligaments are torn or stretched. In addition, there may also be tendons and/or nerve damage.
How is a Shoulder Dislocation Diagnosed?
A dislocated shoulder joint is diagnosed by history, physical examination and an X-ray.
Treatment Options for a Shoulder Dislocation?
Acute shoulder dislocations may reduce spontaneously or require a paramedic or hospital reduction.
Once reduced:
- The shoulder will be immobilized with a sling for several weeks.
- Rehabilitation exercises may be started to restore range of motion, once the pain has subsided.
- Acute surgical repair of torn ligaments, tendons or associated fractures may be considered in certain circumstances.
Shoulder Instability
Acute shoulder dislocations may reduce spontaneously or require a paramedic or hospital reduction.
Once reduced:
- The shoulder will be immobilized with a sling for several weeks.
- Rehabilitation exercises may be started to restore range of motion, once the pain has subsided.
- Acute surgical repair of torn ligaments, tendons or associated fractures may be considered in certain circumstances.
Causes of Shoulder Instability
Any injury to the ligaments that ordinarily stabilise the shoulder can result in shoulder instability. Untreated this can mean pain and loss of confidence in the shoulder, and can lead to in early-onset osteoarthritis in the joint over time.
Shoulder Instability symptoms
- A feeling of the shoulder moving out of place
- Pain
- Recurrent dislocations
- Numbness
To reach the diagnosis, during your consultation your specialist will speak to you about your medical history and take into account any past injuries to the shoulder. They will perform a physical examination and arrange any tests required, these might include X-Rays, CT with 3D reconstruction or MRI scans.
Treating the unstable shoulder
Non-operative measures predominantly aim to restore range of movement to allow for normal shoulder function. Physiotherapy and activity modification can help to alleviate symptoms and prevent future dislocations. When these options have not been successful surgery may be needed.
Labral tears
The ligaments attach to the socket via a strong cartilage ring called the labrum. Importantly, the labrum increases the depth of the socket for greater stability. If excessive force is placed on the arm, the ligaments can pull the labrum off the socket (Bankart Lesion). The ligament may not heal in its normal position, allowing increased movement of the ball on the socket that can predispose to further instability episodes.
SLAP tear(superior-labrum anterior-posterior) is a term that refers to an injury of the top of the labrum, this can involve the biceps tendon muscle attachment. Bankart lesions are labral tears that start below at the middle of the glenoid.
Symptoms of Labral tears
Glenoid labral tears can cause a catching/popping sensation. They may present alongside shoulder instability, and are often painful.
Treatment options for Shoulder Instability
Conservative measures – pain relief, activity modification and physiotherapy can increase the strength of the joint and restore range of movement. If pain persists patients may consider surgical repair of the labral tear and repair of associated surrounding tendons and ligaments if needed.
Instability shoulder surgery
Most shoulder stabilising surgery is performed arthroscopically (key-hole) through small incisions called portals. Your surgeon will have a clear view of your shoulder joint on a magnified television during the operation allowing them to assess the injuries and perform any necessary surgical procedures. Tears can be repaired with sutures and small-specialised bone anchors. Sometimes in difficult instability cases open surgery may be needed, for example when there may be areas of bone loss, these can be treated with a bone graft in a Latarjet procedure. Depending on the injury, your consultant will speak through options with you so that you can participate in shared decision making.
Shoulder stability surgery risks
Shoulder stabilising surgery is a successful operation but like all operations there are some rare complications:
- Anaesthetic risks
- Recurrence of symptoms
- Incomplete resolution of symptoms
- Damage to nerve and blood vessels
- Stiffness
- Haemarthrosis (bleeding into the joint after surgery usually minimal – very rarely requires any further treatment)
- Infection (risk less than 0.5%)
- Chondrolysis (damage to the smooth articular cartilage surface lining of the shoulder joint surface – very rare).
Serious medical problems can lead to ongoing health concerns, prolonged hospitalisation or rarely death. The risk of dying in the operating theatre under anaesthetic is extremely small. For a healthy person having planned surgery, around 1 person may die for every 100,000 general anaesthetics given.
After surgery
Many patients go home the same day with pain relief tablets to take at home. A bandage will be around the operated shoulder and the arm will be in a sling for comfort. The bandage can be removed and the sling should be worn for approximately 6 weeks, but your specialist will make a personalised plan for you and you will receive written post-operative instructions before you are discharged.
Swelling is normal after surgery.
We recommend ice packs be applied to the area for 20 minutes 3-4 times a day until this settles down. You should sleep with a pillow under your elbow whilst you are recovering.
You will be given rehabilitation activities to follow, as well as a clinic appointment to see how you are getting on.
Symptoms of Acromioclavicular joint dislocation
Acromioclavicular joint (AC joint) dislocation – also known as shoulder separation – is where the collarbone (clavicle) comes away from the shoulder blade (acromion). This is common in fit athletic patients with direct trauma during contact sports or a fall onto the shoulder. There are varying degrees of this injury depending on the ligaments sprained and whether the bones are out of alignment.
Acromioclavicular Joint Dislocation
Acromioclavicular joint (AC joint) dislocation – also known as shoulder separation – is where the collarbone (clavicle) comes away from the shoulder blade (acromion). This is common in fit athletic patients with direct trauma during contact sports or a fall onto the shoulder. There are varying degrees of this injury depending on the ligaments sprained and whether the bones are out of alignment.
Symptoms of Acromioclavicular joint dislocation
The patients with this injury may notice a visual deformity compared to the other shoulder. This depends on the degree of severity, without any ligament support the shoulder falls under the weight of the arm and the collarbone (clavicle) is pushed up and appears as a bump on the shoulder. There may also be pain, bruising and swelling, and limited shoulder movement.
Diagnosis
Your consultant will take a history, including finding out about your activity levels and work, examine your shoulder and get an X-ray to check for a fracture and possibly an MRI scan.
Treatment options
In most cases surgery isn’t needed. Pain relief medicines, ice and anti-inflammatories can all help relieve the pain. Immobilising the joint with a sling is also indicated in the acute phase. As the pain settles physiotherapy exercises can restore movement and increase specific strength to stabilize the joint.
Surgery might be needed for severe dislocations where the muscle attachments have been torn, because in these cases local scarring will not be able to provide enough stability in the longer term. Other cases where non-operative measures have failed and patients have ongoing symptoms may also benefit from an operation.
Acromioclavicular joint dislocation surgery
Surgical stabilization of the AC joint can be achieved in a number of ways. This is usually done arthroscopically (key-hole) to improve symptoms. Occasionally a metal plate or may be needed to restore anatomy and/or a ligament reconstruction can be carried out using your own ligaments or synthetic ligaments. Your specialist will talk about the most suitable options for your particular case if surgery is indicated.
Risks of Surgery
Shoulder stabilising surgery is successful, but like all operations, there are some rare complications including anaesthetic risk, infection (superficial or deep) and failure of ligament reconstruction. The specific risks will relate to the technical aspects of the operation you are offered and will be discussed with you in your consultation.
Prognosis after AC joint dislocation
The prognosis is good, whilst some stiffness can remain; most patients make a full recovery and are able to return to work, activity and their sport.
Surrey Orthopaedic Clinic Shoulder Dislocation and ACJ Specialists: